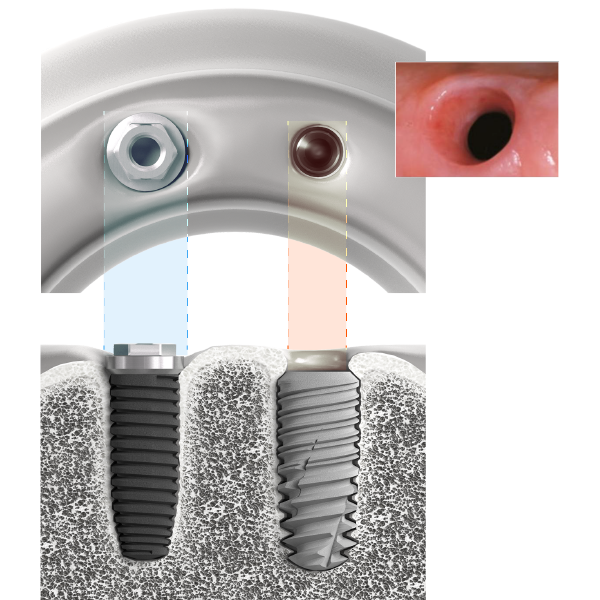
Originally considered a primarily functional solution, today the implant-supported prosthesis is mostly indicated for aesthetic restoration of the anterior region
Immediately visible on smiling, aesthetic restorations are a major challenge as they must take into account surrounding dental tissue (enamel and dentine) as well as periodontal tissue (bone and gum), which may be unpredictable. The aesthetic challenge is all the more complex as the success of this type of restoration is reliant on the subjectivity of the patient.
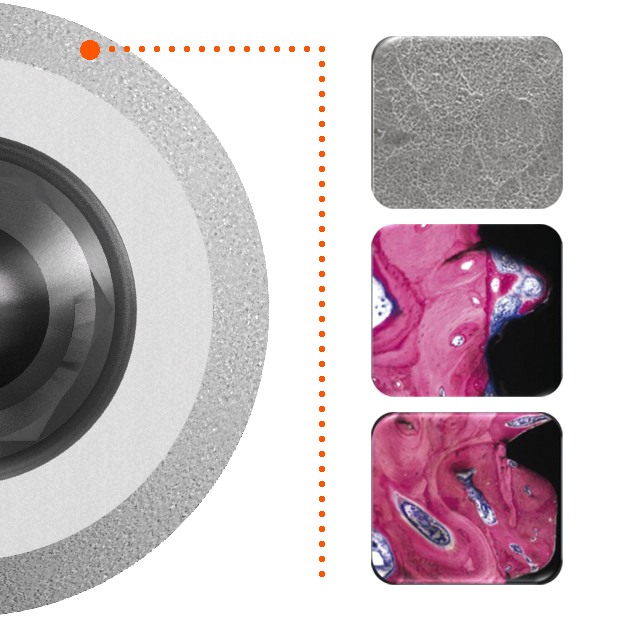
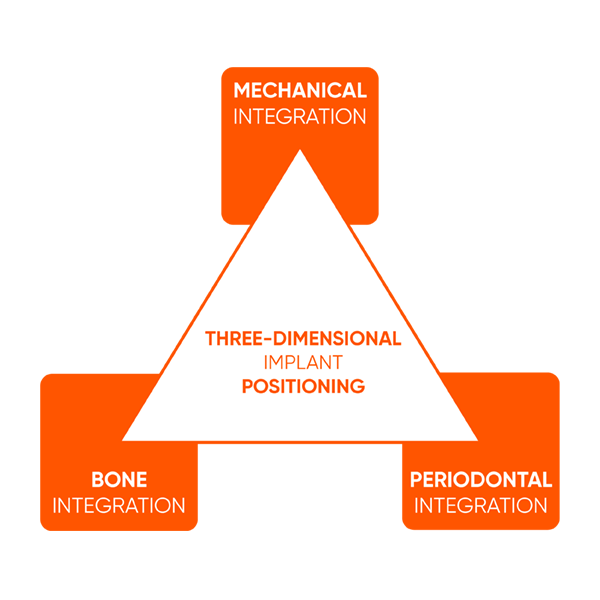
Nevertheless, reconstruction of papillae, jaw alignment, selection of the correct materials and maintenance of periodontal health are universal criteria to be considered when evaluating the reproducibility and permanence of the operative techniques implemented.